Edit has been made to a quote in the section titled “The Fallout” at the end of the piece. A previous quote was removed upon request and instead a direct quote from the New York Times article was used in its place. The quote change does not significantly change the section. 4/2/2024.
Bicalutamide
Bicalutamide is a drug that has never been approved for use in pediatric populations. It is a drug that is taken orally (by mouth) and was approved by the Food and Drug Administration (FDA) as a therapy for men with prostate cancer. It was marketed by AstraZeneca as Casodex, though it is off patent and available as a generic.
When it was first developed and used in the original target population for which it was approved, it was found to have side effects that bothered the men who took it. The men were growing breast tissue. The reason this was happening was because the drug is a nonsteroidal antiandrogen. It blocks testosterone and other androgens from binding to the androgen receptors. The body then gets confused—it knows that it is pumping out testosterone but the receptors that should be receiving that testosterone are reporting back that they have none. So, the body makes more and more testosterone and eventually the body converts that excess testosterone into estrogen and begins to feminize the body.
Bicalutamide, Daniel Schumer in the Journal of Adolescent Medicine writes that the “safety and effectiveness in pediatric patients have not been established by the FDA. Bicalutamide- induced hepatotoxicity is a rare but well-known phenomenon” (Schumer). This is not a drug recognized as part of the standard of care for transgender medicine. Standard of Care Version 8 states, “given that bicalutamide has not been adequately studied in transfeminine populations, we do not recommend its routine use” (Schumer).
I worked in a pediatric transgender center for four and a half years. We were routinely using this drug without oversight by risk management, without oversight by the endocrine division, and without oversight by the Institutional Review Board (IRB). We were using this drug in patients as young as age 14.

Feminizing hormones
Spironolactone (spiro), estrogen, progesterone, and puberty blockers have historically been used in transgender medicine for purposes of feminization. Spiro is also an antiandrogen but it does not fully block the androgen receptors in the same potent way that bicalutamide does. Spiro is also usually taken twice a day, every 12 hours, while bicalutamide is dosed once a day.
Spiro is similar to all other hormones used for cross sex purposes: it has significant side effects that many patients find challenging to deal with. Spiro is a diuretic (sometimes called a “water pill”), which means it causes its users to have an increased need to urinate. Spiro also has significant, well-documented complaints regarding its effects on mental health, including increasing depression, anxiety, brain fog, and memory effects. Spiro is usually combined with estrogen. The endocrinologist in the center I worked in often suggested that bicalutamide simply created better-looking breasts.
Use in pediatric populations
I started working in the pediatric transgender center in July 2018. Bicalutamide was in use when I started. In trainings, no one ever explained that the way we were using it was experimental. I shadowed the endocrinology team and learned about its use and I went on to complete education with patients and families about this drug.
There have been only a small number of papers published on the use of bicalutamide in pediatric transgender care. A search of PubMed produces only 4 total papers, and 1 of the 4 is an editorial about publishing a study on an adolescent patient with bicalutamide-induced hepatotoxity.
In 2024, the Journal of Adolescent Medicine published an editorial that addresses the use of bicalutamide in pediatric patient populations. The author states that, “the largest pediatric study followed 14 boys with familial male limited precocious puberty, a condition with high levels of testosterone production, who were treated with bicalutamide and an aromatase inhibitor for one year. In this study, one participant developed a mild transient transaminitis” (a sign of liver problems) (Schumer).
14 patients.
Another study was a small retrospective study of “23 transfeminine adolescents” to whom “bicalutamide was offered as a second-line agent predominantly after the first-line option (a puberty blocker) was denied for insurance coverage” (Schumer). We were utilizing a drug that was specifically stated in the guidelines to be not standard of care for use in transgender adolescent patients:
When is it research and when is it not
In March of 2019, I drafted my first informed consent document and received Institutional Review Board (IRB) approval for the first research study that we started in the pediatric transgender center. I was still a student at that time in a Master’s of Science Program in Clinical Research Management at the University.
The study was titled, “WUSM Transgender Database.” The purpose was to create a database of patient information. The information collected would be only from patients seeking care at the transgender center and it was meant to include health information, social information, and information reported to the providers.
The study and the approval from the IRB assumed a number of things. The primary assumption was that the medical care being provided met the criteria required for the treatments to qualify as “standard of care.” A research database is considered one of the simplest kinds of studies to get approval for and to manage. There is supposed to be no experimental drug, device, or surgical procedure. It was a simple study for a budding research manager to devise, write, and seek approval for.
In March of 2019, we began consenting patients into the database study (we had not yet created the actual database). The nurse and I completed the consenting process for hundreds of patients.
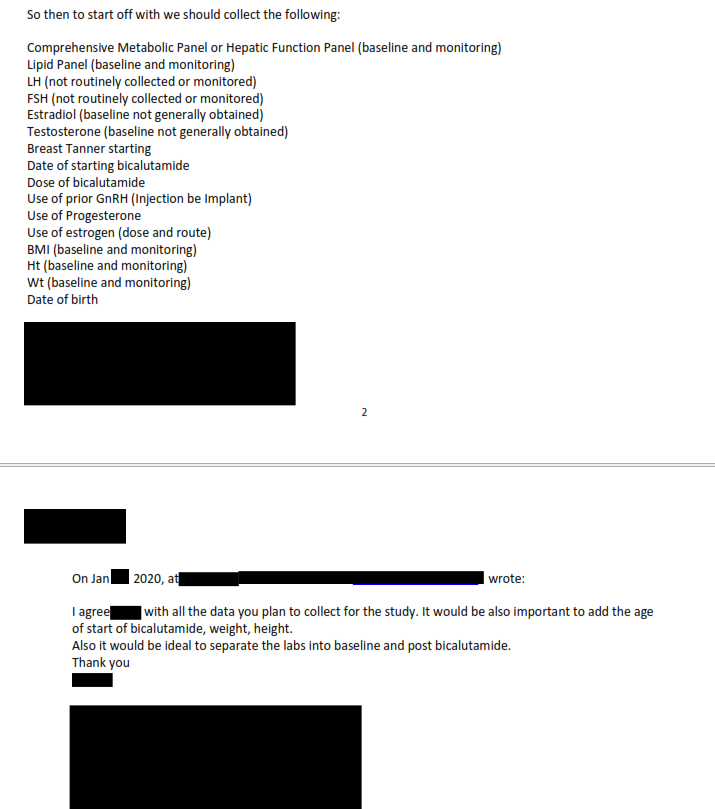
In January of 2020, I was asked to create a subgroup of the patients who had been entered into the database to begin a study within a study (a questionable ethical request itself). This subgroup would be the patients on bicalutamide. Still a student at the time, I continued to work directly with the MDs on this project. Three associate professors in pediatric medicine reviewed all of my work and as a team we began to review this pediatric subgroup.
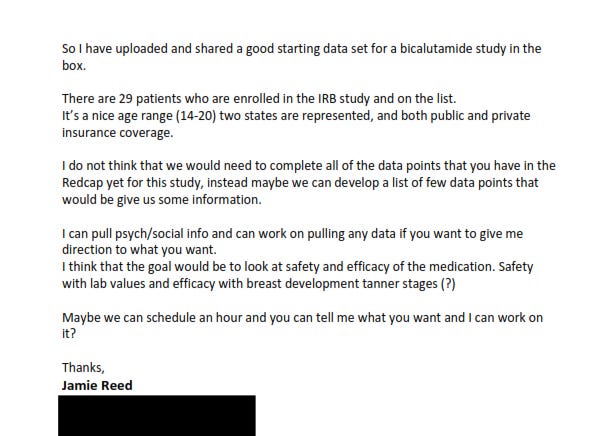
In an email from January 2020, I documented, “there are 29 patients who are enrolled in the IRB study and on the list. It’s a nice age range (14-20) two states are represented, and both public and private insurance coverage.” I went on to write, “I think that the goal would be to look at safety and efficacy of the medication. Safety with lab values and efficacy with breast development tanner stages (?)”
This does not mean that only 29 patients were being given bicalutamide. Rather, this was simply the number of patients who were both on bicalutamide and had been consented into the database study. According to a different spreadsheet I created, there were 103 patients to whom we had given bicalutamide February 2020 and 2022.
Establishing your research questions is the key first step in any project. Clinical trials have four different levels. By clearly documenting that one element we were seeking was “safety ” this could clearly place this as a Phase 1 clinical research question.
A phase one study.
But we had not submitted a protocol to the IRB about the use of bicalutamide, the only thing that we told the IRB was that we wanted to create a database to document the “standard of care” that we were providing patients. The use of bicalutamide itself was never proposed to the IRB as being part of the research question, we told the IRB that the care that we provided was all standard of care.
A phase one study is a small study that is seeking to determine if the drug is safe in the patient population and establish dosing. Phase two is a bit larger and looks at establishing efficacy and any other side effects. Phase two studies are also longer in duration. Phase three is again larger and longer and looks to drill down into efficacy and adverse reactions. Phase four includes the largest number of subjects. According to the FDA, “approximately 70% of drugs” move on from phase one. “Approximately 33% of drugs” move on from phase two and, “25-30% of drugs” move on from phase three.
If it’s experimental, is it research?
Three questions are raised by the use of bicalutamide in this vulnerable patient population. The first question-is bicalutamide the standard of care?- the answer is clearly NO. If it were standard of care, there would be no need to study it in a such a preliminary fashion, as this research would already have been completed and a favorable risk/benefit profile would have been established. So if it is not the standard of care, then is it research or experimental, and is there a difference between the two?
In, Why Human Subjects Research Protection is Important, Michael White addresses these issues while discussing The Belmont Report:
“Research, on the other hand, is defined as “an activity designated to test an hypothesis, permit conclusions to be drawn, and thereby to develop or contribute to generalizable knowledge. This section further expounds on the conflation between the use of the terms experimental and research. When used in reference to a procedure or treatment that significantly deviates from typical (i.e. a treatment that is “new, different, or untested”), the report notes that an “experimental” treatment is not necessarily research. Although they excluded “experimental” treatment from research and the applicable anticipated regulations, the National Commission strongly recommended that such treatments should eventually be incorporated into formal research protocols “to determine if they are safe and effective” The first section of the Belmont Report conclude with the recognition that practice and research may go hand in hand: “the general rule is that if there is any element of research in an activity, that activity should undergo review for the protection of human subjects”
What is clear to me now is that we were providing an experimental treatment to children and adolescents without the safeguards and oversight that research provides. The Belmont Report clearly identifies that experimental treatments need to be incorporated into formal research protocols. What it doesn’t address is what happens when the medical field is giving children and adolescents a treatment that is experimental but could possible not pass muster in getting the protocol to pass the IRB review in a vulnerable patient population.
The Belmont Report was originally drafted in 1978 and is one of the core gospels of clinical research ethics and regulation. It was not the first document written on the subject. Many have heard of or are vaguely aware of the research atrocities that occurred in Nazi Germany. The Nuremberg Code came out in 1947 in response to those atrocities. The Belmont Report followed several decades later and included far more detail and precision. Moral Science: Protecting Participants in Human Subject Research in 2011.
From the Nuremberg Trials, “Twenty-three physicians were indicted, accused of crimes against humanity by conducting criminal scientific and medical experiments on concentration camp prisoners” (White). The physicians tried to argue as part of their defense that there was no applicable laws or regulations on legal versus illegal human research. A memorandum was submitted to the court by two American doctors in which they outlined 6 points defining “legitimate medical research.” These 6 points were expanded to 10 total and they became known as the Nuremberg Code (White).
The Nuremberg Code was brief and it did not address the needs of special populations. These populations include children, prisoners, those with development needs, and pregnant women.
Even before the Nuremberg Codes, the Declaration of Helsinki, and the Belmont Report there was a guidance document that was developed in 1931. This was called the “Circular of the Reich Minister of the Interior” and it was dated from February 1931. In this circular the first guidelines were established, which we have been building on ever since. This guideline directly gets to the heart of our issue- the use of bicalutamide in pediatric gender medicine, and it spells out what should have happened before this drug was ever prescribed.
From the Circular of the Reich Minster of the Interior:
“In order that medical sciences may continue to advance, the initiation in appropriate cases of therapy involving new and as yet insufficiently tested means and procedures cannot be avoided. Similarly, scientific experimentation involving human subjects cannot be completely excluded as such, as this would hinder or even prevent progress in the diagnosis, treatment, and prevention of diseases.”
Innovative therapy, “must be justified and performed in accordance with the principals of medical ethics and the rules of medical practice and theory.”
Innovative therapy, “must assess and examine that the adverse effects which may occur are proportionate to the anticipated benefits”
Innovative therapy, “may be carried out only if it has been tested in advance in animal trials (where these are possible).”
Innovative therapy, “may be carried out only after the subject or his legal representative has unambiguously consented to the procedure in the light of relevant information provided in advance.”
Innovative therapy, “use must be examined with particular care where the subject is a child or person under 18 years of age”
“Exploitation of social hardship in order to undertake innovative therapy is incompatible with the principals of medical ethics”
Adult versus Pediatrics
At a certain point in 2021- 2022 it became clear that we needed to start shifting more patients from pediatric care to adult care simply due to the volume of patients. When we first opened as a center we were publicly stating that we would see patients until the age of 26. That became an untenable age range to continue to treat and the adult center had finally opened.
Initially, the adult center had a less then stellar relationship with the activist community, but eventually they reached a point where they had received the activist community’s blessing and we were given the green light to transfer our patients to the adult center at an earlier and earlier age. This shift meant a closer relationship with the adult providers and it was around this time that I came to understand more clearly the situation regarding bicalutamide.
The adult center was not routinely using this drug and they cited the known toxicity as one of the reasons. This was concerning for me clinically because it meant that a drug that my clinic was considered safe to use in a pediatric population was not considered safe by clinicians working with an adult population.
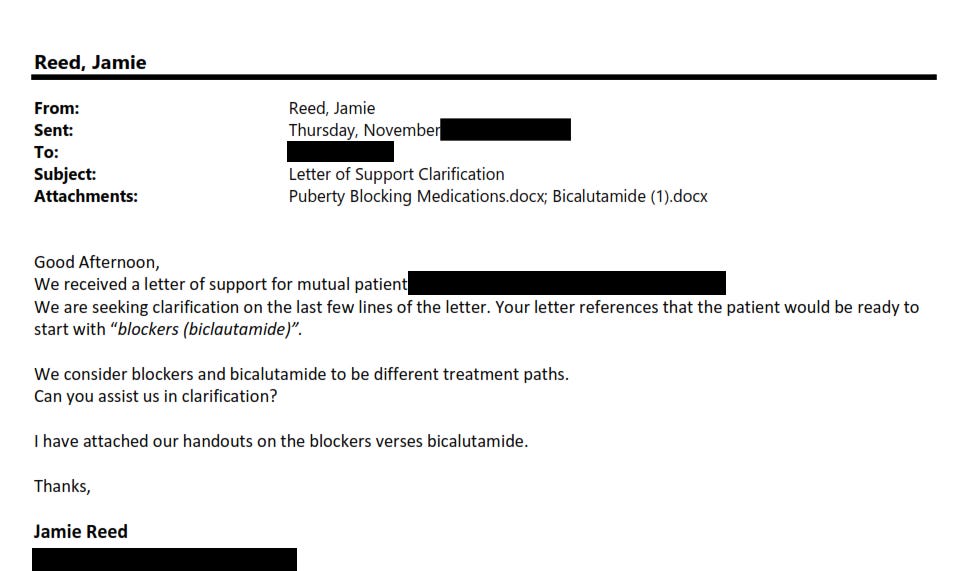
Another issue that had been present since 2019 but had gotten so prevalent that it was a common topic of discussion was that patients and their families did not understand this drug. As seen in the email from a prominent therapist in 2019, the drug was seen and referred to, incorrectly, as a “blocker.”
Blocker versus cross sex hormone
This common confusion was troubling and is similar to something that was raised in the WPATH files. These are complex treatments that have a long list of known and suspected effects and side effects. Parents would state that they were consenting for their child to start a blocker. This was sort of true-but not really. This was a drug that did not merely block puberty but also caused feminization. This would be equivalent to a natal female starting testosterone.
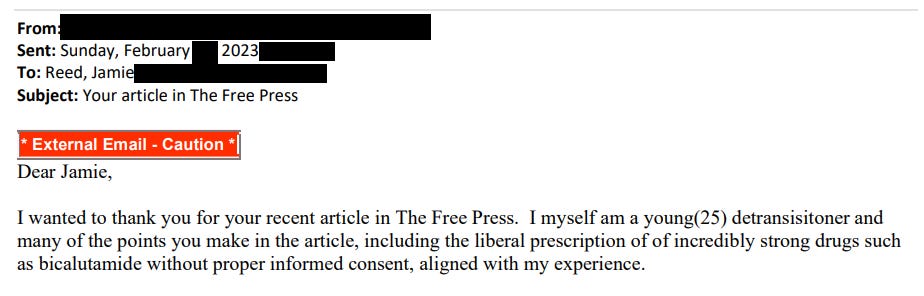
Patients had started calling this drug their “mini blocker,” which was also troubling. This was not mini in any way and this was not just blocking. I had a conversation (maybe better characterized as my getting yelled at by a parent) outside of court in Missouri. I was standing and speaking with Azeen Ghorayshi from the NYT. In a similar troubling situation this parent also called this drug a blocker and when I attempted to explain that this characterization was incorrect the parent informed me that their child understood its mechanism and therefore all was well. I was scared being yelled at and having car doors slammed. So much anger. But this interaction simply drilled home that a good, informed consent process requires that the parent who consented can, at a minimum, teach back the basics of what drug they consented to their child taking.
As the pressures inside the center grew and as the conflicts over the care increased, bicalutamide was always a part of the equation. As I finished my studies, I became more convinced that we were conducting medical research, especially regarding bicalutamide outside of any IRB oversight and without any of the safety monitoring or reporting requirements that IRB oversight brings.
I left the center in the Fall of 2022 and remained in almost daily contact with the nurse in the center. She was privy to every step of the drafting of the affidavit and the letter to the attorney general. She told me stories and continued to express her concerns about what was happening in the center when we spoke on the phone and texted.
The patient in the affidavit
The nurse told me the story of the patient in the winter of 2022. She didn’t share the patient’s name, or DOB, or Medical Record Number (MRN). And as she told it to me she had an interaction with a Mom who was very upset because their child had liver damage and was told by the renal department to stop taking bicalutamide. We were not surprised one bit; we had been anticipating that this would happen. The nurse also told me that in the interaction the parent had threatened to sue.
This patient story was added to the affidavit because it highlighted that the use of this drug was completely outside of any and all guidelines. And I trusted the nurse as we had worked together for years. It was an important story, out of all of the stories. It was another patient that the hospital let fall into the huge crack we created for these kids.
We have the NYT to thank for more of the details of this specific case, but that was never my hope. I hoped (I still do) that the hospital would have completed a detailed investigation. I hoped that the hospital also would have provided the redacted records to the relevant state health authorities as requested for an independent investigation.
My affidavit was not the record of an investigation. My affidavit was simply an attempt to say to the world- “hey, please, someone please look over here. Please count every child. Please review their records, and not just this patient who experienced liver damage. Look at all of them.” I did my best to count as many as I could, to produce what I could, but I truly expected a real investigation to occur.
The fallout
Many have complained about the inclusion of this case in the affidavit. Some of the complaints stated that the liver damage could have been due to something other than bicalutamide: “she was immunocompromised, and experienced liver problems only after getting COVID and taking another drug with possible liver side effects” (Ghorayshi). If the patient was being treated with bicalutamide on a research protocol, and that protocol acknowledged the clearly known risk to the liver, then the protocol would have clear stipulations that other treatments that risk liver damage either need to be avoided or that the bicalutamide would be stopped.
In addition, the research protocol would have increased lab tests for liver function and would have a mechanism to report all adverse and serious adverse effects while on drug. While it is true that the COVID infection itself could have been a contributing factor to the liver damage, “the etiopathogenesis of liver damage related to direct COVID-19 infections has not been completely determined yet. However, it is hypothesized to be direct hepatocellular damage, as is observed by the elevation in the cytonecrosis enzymes levels” (Saha). But it is also noted that, “Liver disorders in COVID-19 patients using several concomitant off-label drugs (potentially causing further liver damage) should be a warning sign for rapid identification and early intervention.” (Saha).
The research protocol should also have attempted to reduce the risk of other drugs being used that are known to cause liver damage because it is known, “as the evidence of drug-induced liver injury (DILI) concerning various drugs is often large and scattered across multiple disciplines, it becomes difficult for clinicians and researchers to search for evidence related to each drug.” Hence, in a phase one study the other drugs would be eliminated or part of the screening processes for study eligibility (Saha).
We prescribed a drug that should not have been used in this patient population outside of IRB review and we harmed young people along the way. My concerns have not diminished. They have only grown as I learn more from those across this nation:
____________________________________________________________________________
Works Cited
Ghorayshi, Azeen. How a Small Gender Clinic Landed in a Political Storm. New York Times. August 23, 2023.
London, Alex John. The Ambiguity and the Exigency: Clarifying ‘Standard of Care’ Arguments in International Research. Journal of Medicine and Philosophy. Vol. 25, No. 4, pp 379-397. 2000.
Saha, Lekha. Soumya Vij, Kajal Rawat. Liver Injury induced by COVID-19 treatment- what do we know? World Journal of Gastroenterology. 28 (45): 6314-6327. 2022.
Schumer, Daniel. Roberts, Stephanie. Placing a Report of Bicalutamide-Induced Hepatotoxicity in the Context of Current Standards of Care for Transgender Adolescents. Journal of Adolescent Health 74: 5-6. 2024.
White, Michael. Why Human Subjects Research Protection is Important. Ochsner Journal 20: 16-33. 2020.






These posts are very helpful in understanding the operation of the clinic, but might I suggest that, if possible, you try to find a medical consultant to review the medical information? For example, "mild transient transaminitis" is a sign of liver stress but not usually actual liver problems and is quite a common side effect of many medications, including quite a number that are used for mental health conditions. It is also quite common when people have a virus such as mono or even a flu-like virus. In fact, if there is no other obvious cause, the patient has no other symptoms of liver disease and they are generally young-ish and in reasonably good health, mild transient transaminitis is often assumed to have been caused by a virus with minimal to no other workup. It can also happen after a night of heavy drinking. Generally speaking, a patient who develops mild transaminitis is monitored through blood testing. They may or may not switch to a different drug depending on their and the doctors' discretion. However, if the transaminitis resolves relatively quickly, as "transient" would suggest, generally you stay on course. Transaminitis that is relatively mild or even moderate but resolves on its own is not considered a liver problem or even a serious side effect. In fact, there is a decent likelihood that if the one out of 14 patients who developed it continued the drug and it still resolved, that it wasn't caused by the drug at all, or that the drug was just one in a number of factors predisposing the kid to having this transient bump in liver enzymes in his bloodwork.
The point being, that just because this one kid in the study developed it does not mean it was related to the drug and also does not necessarily indicate that it was a real problem. This is why it can be difficult for lay people to fully interpret medical research, even if they faithfully Google every single term they don't know. There is simply a lot of context missing. Coming from a health care background, I personally would find these posts more convincing if the medical info was more accurate. Otherwise, it gives the whole thing a veneer of alarmism, and I think you have some very important things to say. I think it's essential that there is more transparency in this field-at a minimum-and you are well-placed to provide it. I fully recognize the difficulty in discussing medical issues without a medical background, and that is why it would in my opinion reach a broader audience more effectively if you had a medical consultant to review the strictly medical info that is needed to provide context for what you're saying. I don't think it helps anyone to increase the amount of half-truths or out of context statements floating around in this area, and you're far from the only commentator to make some mistakes in this regard. But imo ANY inaccuracy just makes it easier for people with bad intentions to discredit everything you say, and that would be really unfortunate. Of course, I'm just one person.
In any case, thank you for taking the time to distribute your knowledge.
Very informative. Thanks Jamie and LGBTCC!